Home / Intelligence / Blog / Are Current Reimbursement Options for Opioid Use Disorder DTx Causing a Barrier to Widespread Adoption in the USA?
Published November 9, 2021
In 2020, Trinity assessed three applications developed to treat Opioid Use Disorders (OUD) (e.g., reSET-O, Connections, DynamiCare) through the lens of ICER conducting a cost-effectiveness evaluation. Only a year later, several more health tech startups have adopted a preventative outlook and seek to address chronic pain with digital health tools (e.g., phone applications). A key focal point is the current public health issue faced by the US with ~2.1 million Americans diagnosed with OUD.
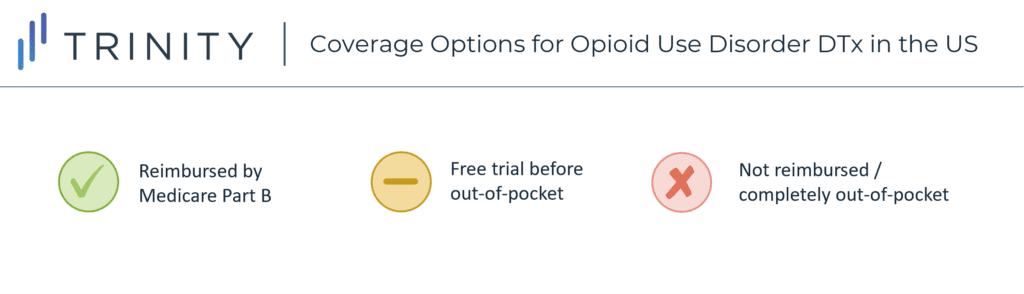
These applications, including Clearing, Curable, Remedee Labs, Swing Therapeutics and AppliedVR, seek to proactively reduce the number of patients using painkillers to address chronic pain through a diverse range of techniques, from biopsychosocial methods to electromagnetic waves. When looking at each tool’s revenue model, they all rely on a long-term subscription, but insurance reimbursement differs significantly between products and their components, potentially posing a barrier to widespread adoption.
As these applications seek insurance reimbursement, we anticipate real-world evidence proving efficacy and downstream cost offsets to be pivotal for success.
By Crystal Zhao and Kate Watkins
Related Intelligence
Blog
ISPOR 2023 Trinity Panel: Enabling Patient Access to Digital Therapeutics – The Optimal Approach?
Monica Martin de Bustamante, Sr. Partner of Trinity’s Evidence, Value, Access, and Pricing (EVAP) team, moderated an exciting conversation at ISPOR 2023 Global in Boston earlier this month. Monica spoke with Lisa Marsch, Ph.D., Benjamin Parcher, PharmD, MS, and Fulton Velez, MD, MS, MBA, all experts in the field of Digital Therapeutics (DTx), about the […]
Read More
Webinars
Payer Predictions: Evolution of the U.S. Digital Therapeutics Reimbursement Landscape
Available On Demand
The digital therapeutics (DTx) market is growing rapidly, but a lack of clarity around their reimbursement framework in the U.S. means that there is limited coverage. DTx developers— and pharmaceutical organizations seeking an integrated digital offering— are left to wonder how the payer landscape will evolve as they strategize for the future. Join Trinity Life […]
Watch Now
White Papers
Reimbursement of Digital Therapeutics in the U.S.
Digital therapeutics (DTx) are impacting how patients are treated, interact with their providers and think about their own health. DTx have garnered interest from the investment community as well as pharma companies seeking an integrated digital offering. However, payers have not yet established a clear framework for integrating these technologies in their plans. Coverage of […]
Read More
